Arizona Medicaid (AHCCCS) Promoting Interoperability (PI) Program for Eligible Professionals
If you have any questions about the AHCCCS Promoting Interoperability (PI) Program (formerly the Medicaid EHR Incentive Program), Health Current is available to provide educational assistance and support for the PI Program. Contact us at 602-688-7210 or via email at ehr@healthcurrent.org.
Download 2021 PI Webinars Flyer Here
The Medicaid Promoting Interoperability Program for Eligible Professionals (EPs) is an incentive program open to Arizona providers who meet eligibility requirements. Annually EPs may elect to participate in the program by submitting proof of their eligibility to AHCCCS and attesting through Arizona’s Electronic Provider Incentive Payment (ePIP) System to meeting the performance requirements for the program year. After eligibility and performance submissions are reviewed by AHCCCS, EPs who attest successfully and meet the program requirements receive a lump sum incentive payment.
The Medicaid Promoting Interoperability program began in 2011 as the Medicaid EHR Incentive Program and continues through 2021. EPs may claim a maximum of six incentive payments over the life of the program and must have received at least one payment during Program Years 2011 through 2016 to continue participation after 2016. Providers are not required to notify AHCCCS if they decide to skip a program year, as participation is optional and there is no penalty for non-participation.
The Arizona Medicaid Program does not allow third party attestation for Eligible Providers in the Electronic Provider Incentive Payment System (ePIP). Eligible Providers should actively participate in the ePIP attestation process and are responsible for the completeness and accuracy of the information in their attestation. Providers may claim eligibility either individually or as part of an organization, but all EPs attest individually to meeting performance requirements.
Eligible Professionals directing their incentive payment to their organization must be affiliated with that organization at the time of attestation.
Eligibility
Eligible Professionals (EPs) include Physicians, Nurse Practitioners, Certified Nurse-Midwives and Dentists. Physician Assistants who practice in a Federally Qualified Health Center or Rural Health Clinic led by a Physician Assistant are also eligible.
EPs applying for years two through six must meet one of the following criteria:
- Have a minimum 30% Medicaid patient volume to claim an incentive payment of $8,500
- Have a minimum 20% Medicaid patient volume and be credentialed as a pediatrician to claim an incentive payment of $5,667.
- Practice predominately in a Federally Qualified Health Center or Rural Health Clinic and have a minimum 30% Medicaid/Needy patient volume to claim an incentive payment of $8,500.
- Practice predominately in a Federally Qualified Health Center or Rural Health Clinic, have a minimum 20% Medicaid/Needy patient volume and be credentialed as a pediatrician to claim an incentive payment of $5,667.
In Arizona, encounter information from any consecutive 90 days in the calendar year prior to the program year is used to calculate the Medicaid or Needy Patient Volumes identified above. For example, providers attesting for program year 2020 would use encounter information from calendar year 2019 to prove eligibility.
EPs must already have received at least one incentive payment for a program year prior to 2017 to continue participation.
General Requirements
Beginning in 2019, all eligible professionals (EPs) are required to use 2015 edition certified electronic health record technology (CEHRT) to meet the requirements of the Promoting Interoperability (PI) Program. The 2015 Edition CEHRT does not have to be implemented on January 1st. However, the functionality must be in place by the first day of the Promoting Interoperability reporting period and the product must be certified to the 2015 Edition criteria by the last day of the reporting period. In some situations, the product may be deployed but pending certification.
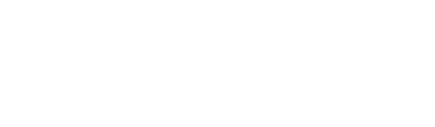
Changes in Registration
CMS maintains a registration record for all Eligible Professionals participating in the program. EPs needing to change their program registration information may do so at https://ehrincentives.cms.gov/hitech/loginCredentials.action.
Reporting Period
In 2019, Eligible Professionals will attest to two categories of measures:
- Medicaid Promoting Interoperability Program Eligible Professionals Objectives and Measures (PI Measures). EPs report their performance on these measures for any consecutive 90 days in 2019.
- Electronic Clinical Quality Measures (eCQMs). Returning EPs who have previously attested to Meaningful Use have a one-year eCQM reporting period. First-time Meaningful Use attesters have a 90-day eCQM reporting period.
Attestation
Please consult the Attestation Deadline information on the AHCCCS web site for the latest information on the attestation period for Program Year 2019.
The attestation period takes place during the calendar year after the program year. EPs attesting for Program Year 2019 will submit their attestations during 2020.
Promoting Interoperability (PI) Objectives and Measure
The PI Objectives and Measures for 2019 are the previously established Meaningful Use Stage 3 Objectives and Measures as modified by the 2019 Medicare Physician Fee Schedule Final Rule. There are 8 Objectives containing 20 measures. For a listing of Objectives, see 2019 Objectives and Measures. Click on the Name of each Objective to retrieve the detailed specifications for each measure included in the Objective.
| Promoting Interoperability Objective | Number of Measures | |
|---|---|---|
| 1 | Protect Patient Health Information | 1 |
| 2 | Electronic Prescribing (eRx) | 1 |
| 3 | Clinical Decision Support (CDS) | 2 |
| 4 | Computerized Provider Order Entry (CPOE) | 3 |
| 5 | Patient Electronic Access | 2 |
| 6 | Coordination of Care | 3 |
| 7 | Health Information Exchange | 3 |
| 8 | Public Health Reporting | 5 |
The documentation for each Objective specifies how many of the measures must be attested and which measures have exclusions available. Generally, EPs must either meet the threshold for passing the measure or qualify for an exclusion to attest successfully.
Electronic Clinical Quality Measures (eCQMs)
Eligible Professionals are required to report on any six eCQMs related to their scope of practice. At least one measure reported must be an outcome measure, if any are relevant. If no outcome measures are relevant to that EP, at least one measure reported must be a high-priority measure. If there are no outcome or high priority measures relevant to an EP’s scope of practice, they must report on any six relevant measures.
Outcome Measures for 2019
| Measure Title | CMS eCQM ID | eCQM NQF | NQF | Quality Number | Measure Type | MIPS High Priority |
|---|---|---|---|---|---|---|
| Diabetes: Hemoglobin A1c (HbA1c) Poor Control (>9%)* | CMS122v7 | None | 59 | 1 | Intermediate Outcome | X |
| Cataracts: Complications within 30 Days Following Cataract Surgery Requiring Additional Surgical Procedures | CMS132v7 | None | 564 | 192 | Outcome | X |
| Cataracts: 20/40 or Better Visual Acuity within 90 Days Following Cataract Surgery | CMS133v7 | None | 565 | 191 | Outcome | X |
| Controlling High Blood Pressure* | CMS165v7 | None | 18 | 236 | Intermediate Outcome | X |
| Depression Remission at Twelve Months | CMS159v7 | 0710e | 710 | 370 | Outcome | X |
| Children Who Have Dental Decay or Cavities | CMS75v7 | None | None | 378 | Outcome | X |
*Included in the 2018 Medicaid and CHIP Core Measure Sets
All Outcome Measures are High Priority Measures. See the table below for the additional High Priority Measures not considered Outcome Measures. Measures may be designated as High Priority either by MIPS Quality Payment Program or by inclusion in the Medicaid and CHIP Core Measure Sets. Providers with both Medicare and Medicaid patient populations may prefer to choose measures considered High Priority by both programs.
Additional High Priority Measures for 2019
| Measure Title | CMS eCQM ID | eCQM NQF | NQF | Quality Number | Measure Type | MIPS High Priority |
|---|---|---|---|---|---|---|
| Appropriate Testing for Children with Pharyngitis | CMS146v7 | None | None | 66 | Process | X |
| Appropriate Treatment for Children with Upper Respiratory Infection (URI) | CMS154v7 | None | 69 | 65 | Process | X |
| Appropriate Use of DXA Scans in Women Under 65 Years Who Do Not Meet the Risk Factor Profile for Osteoporotic Fracture | CMS249v1 | None | None | 472 | Process | X |
| Child and Adolescent Major Depressive Disorder (MDD): Suicide Risk Assessment | CMS177v7 | 1365e | None | 382 | Process | X |
| Closing the Referral Loop: Receipt of Specialist Report | CMS50v7 | None | None | 374 | Process | X |
| Diabetic Retinopathy: Communication with the Physician Managing Ongoing Diabetes Care | CMS142v7 | None | 89 | 19 | Process | X |
| Documentation of Current Medications in the Medical Record | CMS68v8 | None | 419 | 130 | Process | X |
| Falls: Screening for Future Fall Risk | CMS139v7 | None | 101 | 318 | Process | X |
| Functional Status Assessment for Total Hip Replacement | CMS56v7 | None | None | 376 | Process | X |
| Functional Status Assessment for Total Knee Replacement | CMS66v7 | None | None | 375 | Process | X |
| Functional Status Assessments for Congestive Heart Failure | CMS90v8 | None | None | 377 | Process | X |
| Initiation and Engagement of Alcohol and Other Drug Dependence Treatment* | CMS137v7 | None | 4 | 305 | Process | X |
| Oncology: Medical and Radiation - Pain Intensity Quantified | CMS157v7 | None | 384 | 143 | Process | X |
| Prostate Cancer: Avoidance of Overuse of Bone Scan for Staging Low Risk Prostate Cancer Patients | CMS129v8 | None | 389 | 102 | Process | X |
| Use of High-Risk Medications in the Elderly | CMS156v7 | None | 22 | 238 | Process | X |
| Breast Cancer Screening* | CMS125v7 | None | 2372 | 112 | Process | |
| Anti-depressant Medication Management* | CMS128v7 | None | 105 | 9 | Process | |
| Follow-up Care for Children Prescribed ADHD Medication (ADD)* | CMS136v8 | None | 108 | 366 | Process | |
| Chlamydia Screening for Women* | CMS153v7 | None | 33 | 310 | Process | |
| Weight Assessment and Counseling for Nutrition and Physical Activity for Children and Adolescents* | CMS155v7 | None | 24 | 239 | Process | |
| Preventive Care and Screening: Screening for Depression and Follow-up Plan* | CMS2v8 | None | 418 | 134 | Process |
* Included in the 2018 Medicaid and CHIP Core Measure Sets
Eligible Professionals should review their CEHRT to verify which measures are available in their system. Not all systems can provide all measures and providers may need to work with their vendor to determine the best set of measures to report. If the CEHRT has a different version of the measure than is currently specified, EPs may still report the measure for the Medicaid PI Program if the reporting format of the measure has not changed. Because of variabilities in systems, measures and relevance to providers, it is a best practice to track all available measures and select six relevant measures for attestation in ePIP.
The list of available eCQMs for EPs in 2019 is aligned with the list of eCQMs for Eligible Clinicians participating in the Medicare Quality Payment Program MIPS and/or the e-specified measures included in the 2018 Medicaid and CHIP Core Measure Sets. A list of these eCQMs can be found at https://ecqi.healthit.gov/ep-ec-ecqms by selecting 2019 as the Performance/Reporting period and downloading the Eligible Clinicians and Eligible Professionals Table of eCQMs. All eCQMs in the Core Sets are considered high priority measures for the Medicaid Promoting Interoperability Program but may or may not also be considered high priority measures for MIPS.
Note: There is no performance scoring on eCQMs in the Medicaid program. While CMS advises reporting on measures containing numerators and denominators before reporting on measures containing zeros, zero is an acceptable result provided that this value was produced by certified EHR technology. CMS and AHCCCS strongly encourage providers to report CQMs relevant to their patient population.
Reporting Period
In 2020, Eligible Professionals will attest to two categories of measures:
- Medicaid Promoting Interoperability Program Eligible Professionals Objectives and Measures (PI Measures). EPs report their performance on these measures for any consecutive 90 days in 2020.
- Electronic Clinical Quality Measures (eCQMs). EPs report their performance on these measures for any consecutive 90 days in 2020. The reporting period is a minimum, and EPs are encouraged to report on a longer period if they can do so.
- Download the Arizona Medicaid Promoting Interoperability (PI) Program Eligible Professional Meaningful Use Checklist for Program Year 2020 Stage 3.
Attestation
Please consult the Attestation Deadline information on the AHCCCS web site for the latest information on the attestation period for Program Year 2020.
The attestation period takes place during the calendar year after the program year. EPs attesting for Program Year 2020 will submit their attestations during 2021.
Promoting Interoperability (PI) Objectives and Measures
The PI Objectives and Measures for 2020 are the previously established Meaningful Use Stage 3 Objectives and Measures as modified by the 2019 Medicare Physician Fee Schedule Final Rule. There are 8 Objectives containing 20 measures. For a listing of Objectives, see 2020 Objectives and Measures. Click on the Name of each Objective to retrieve the detailed specifications for each measure included in the Objective.
| Promoting Interoperability Objective | Number of Measures | |
|---|---|---|
| 1 | Protect Patient Health Information | 1 |
| 2 | Electronic Prescribing (eRx) | 1 |
| 3 | Clinical Decision Support (CDS) | 2 |
| 4 | Computerized Provider Order Entry (CPOE) | 3 |
| 5 | Patient Electronic Access to Health Information | 2 |
| 6 | Coordination of Care through Patient Engagement | 3 |
| 7 | Health Information Exchange | 3 |
| 8 | Public Health and Clinical Data Registry Reporting | 5 |
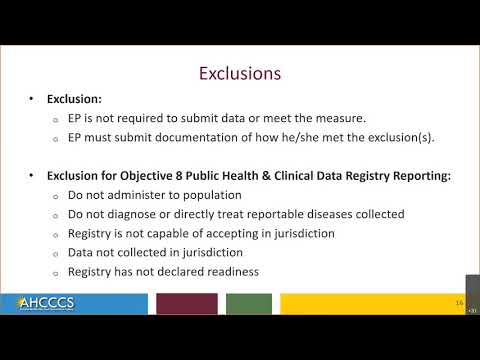
The documentation for each Objective specifies how many of the measures must be attested and which measures have exclusions available. Generally, EPs must either meet the threshold for passing the measure or qualify for an exclusion to attest successfully.
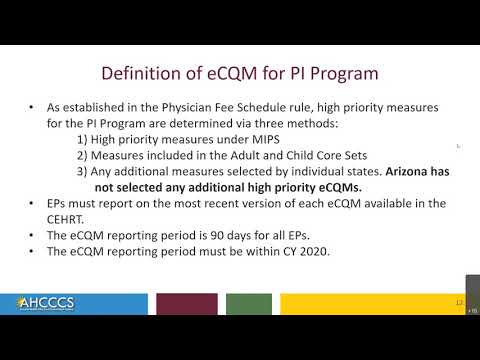
Electronic Clinical Quality Measures (eCQMs)
Eligible Professionals are required to report on any six eCQMs related to their scope of practice. At least one measure reported must be an outcome measure, if any are relevant. If no outcome measures are relevant to that EP, at least one measure reported must be a high-priority measure. If there are no outcome or high priority measures relevant to an EP’s scope of practice, they must report on any six relevant measures.
Outcome Measures for 2020
| Measure Title | CMS eCQM ID | eCQM NQF | NQF | Quality Number | Measure Type | MIPS High Priority |
|---|---|---|---|---|---|---|
| Diabetes: Hemoglobin A1c (HbA1c) Poor Control (>9%)* | CMS122v8 | N/A | 59 | 1 | Intermediate Outcome | X |
| Cataracts: 20/40 or Better Visual Acuity within 90 Days Following Cataract Surgery | CMS133v8 | 0565e | 565 | 191 | Outcome | X |
| Controlling High Blood Pressure* | CMS165v8 | None | 18 | 236 | Intermediate Outcome | X |
| Depression Remission at Twelve Months | CMS159v8 | 0710e | 710 | 370 | Outcome | X |
| Children Who Have Dental Decay or Cavities | CMS75v8 | None | None | 378 | Outcome | X |
| International Prostate Symptom Score (IPSS) or American Urological Association-Symptom Index (AUA-SI) Change 6-12 Months After Diagnosis of Benign Prostatic Hyperplasia | CMS771v1 | None | None | 476 | Patient Reported Outcome | X |
* Included in the 2019 Medicaid and CHIP Core Measure Sets
All Outcome Measures are High Priority Measures. See the table below for the additional High Priority Measures not considered Outcome Measures.
Additional High Priority Measures for 2020
| Measure Title | CMS eCQM ID | eCQM NQF | NQF | Quality Number | Measure Type | MIPS High Priority |
|---|---|---|---|---|---|---|
| Diabetic Retinopathy: Communication with the Physician Managing Ongoing Diabetes Care | CMS142v8 | 0089e | 89 | 19 | Process | X |
| Appropriate Treatment for Children with Upper Respiratory Infection (URI) | CMS154v8 | None | 69 | 65 | Process | X |
| Appropriate Testing for Children with Pharyngitis | CMS146v8 | None | None | 66 | Process | X |
| Prostate Cancer: Avoidance of Overuse of Bone Scan for Staging Low Risk Prostate Cancer Patients | CMS129v9 | 0389e | 389 | 102 | Process | X |
| Documentation of Current Medications in the Medical Record | CMS68v9 | 0419e | 419 | 130 | Process | X |
| Oncology: Medical and Radiation Pain Intensity Quantified | CMS157v8 | 0384e | 384 | 143 | Process | X |
| Use of High-Risk Medications in the Elderly | CMS156v8 | None | 22 | 238 | Process | X |
| Initiation and Engagement of Alcohol and Other Drug Dependence Treatment | CMS137v8 | None | None | 305 | Process | X |
| Falls: Screening for Future Fall Risk | CMS139v8 | None | 101 | 318 | Process | X |
| Closing the Referral Loop: Receipt of Specialist Report | CMS50v8 | None | None | 374 | Process | X |
| Functional Status Assessment for Total Knee Replacement | CMS66v8 | None | None | 375 | Process | X |
| Functional Status Assessment for Total Hip Replacement | CMS56v8 | None | None | 376 | Process | X |
| Functional Status Assessments for Congestive Heart Failure | CMS90v9 | None | None | 377 | Process | X |
| Child and Adolescent Major Depressive Disorder (MDD): Suicide Risk Assessment | CMS177v8 | 1365e | None | 382 | Process | X |
| Appropriate Use of DXA Scans in Women Under 65 Years Who Do Not Meet the Risk Factor Profile for Osteoporotic Fracture | CMS249v2 | None | None | 472 | Process | X |
| Breast Cancer Screening* | CMS125v8 | None | 2372 | 112 | Process | |
| Cervical Cancer Screening* | CMS124v8 | None | None | 309 | Process | |
| Childhood Immunization Status* | CMS117v8 | None | None | 240 | Process | |
| Chlamydia Screening for Women | CMS153v8 | None | None | 310 | Process | |
| Follow-Up Care for Children Prescribed ADHD Medication (ADD) * | CMS136v9 | None | None | 366 | Process | |
| Weight Assessment and Counseling for Nutrition and Physical Activity for Children and Adolescents* | CMS155v8 | None | None | 239 | Process |
* Included in the 2019 Medicaid and CHIP Core Measure Sets
Eligible Professionals should review their CEHRT to verify which measures are available in their system. Not all systems can provide all measures and providers may need to work with their vendor to determine the best set of measures to report. If the CEHRT has a different version of the measure than is currently specified, EPs may still report the measure for the Medicaid PI Program if the reporting format of the measure has not changed. Because of variabilities in systems, measures and relevance to providers, it is a best practice to track all available measures and select six relevant measures for attestation in ePIP.
The list of available eCQMs for EPs in 2020 is aligned with the list of eCQMs for Eligible Clinicians participating in the Medicare Quality Payment Program MIPS and/or the e-specified measures included in the 2019 Medicaid and CHIP Core Measure Sets. A list of these eCQMs can be found at https://ecqi.healthit.gov/ep-ec-ecqms by selecting 2020 as the Performance/Reporting period and downloading the Eligible Clinicians and Eligible Professionals Table of eCQMs. All eCQMs in the Core Sets are considered high priority measures for the Medicaid Promoting Interoperability Program but may or may not also be considered high priority measures for MIPS.
Note: There is no performance scoring on eCQMs in the Medicaid program. While CMS advises reporting on measures containing numerators and denominators before reporting on measures containing zeros, zero is an acceptable result provided that this value was produced by certified EHR technology. CMS and AHCCCS strongly encourage providers to report CQMs relevant to their patient population.
The Promoting Interoperability and eCQM reporting periods for Medicaid EPs in 2021 will be a minimum of any continuous 90-day period within the 2021 Calendar Year (CY). Because all program payments are legislatively mandated to occur by 12/31/2021, the end date for an EP’s reporting period in 2021 must fall before October 31, 2021. This truncated reporting period is needed to facilitate payment processing by the end of 2021.
Medicaid EPs may conduct a security risk analysis at any time during CY 2021, even if the EP conducts the analysis after the EP attests to meaningful use of CEHRT to the state. A Medicaid EP who has not completed a security risk analysis for CY 2021 by the time he or she attests to meaningful use of CEHRT for CY 2021 will be required to attest that he or she will complete the required analysis by December 31, 2021. This allows for maximum flexibility for Medicaid EPs to attest before their state’s 2021 deadline, while maintaining their annual SRA schedule.
All Medicaid Promoting Interoperability payments to EPs must be issued by December 31, 2021.
Federal support to the states for administrative activities related to audits and appeals is available through September 30, 2023.
2021 PI Program Webinar Series
Open Forum Documentation Requirements Program Closure – September
- Final AHCCCS Open Forum Documentation Presentation – September 16, 2021
- Final AHCCCS Open Forum Program Closure Presentation – September 16 2021
Open Forum for Meaningful Use Focus: Electronic Prescribing, Clinical Decision Support, and Computerized Provider Order Entry – August
AHCCCS Open Forum Presentation – August 26 2021_Poll

Open Forum: Objective 5 Patient Electronic Access Objective 6 Coordination of Care – July
- AHCCCS Patient Electronic Access and Coordination of Care Open Forum – July 29, 2021
- AHCCCS Program Year 2021 – Coordination of Care through Patient Engagement Frequently Asked Questions
- AHCCCS Program Year 2021 – Patient Electronic Access Frequently Asked Questions

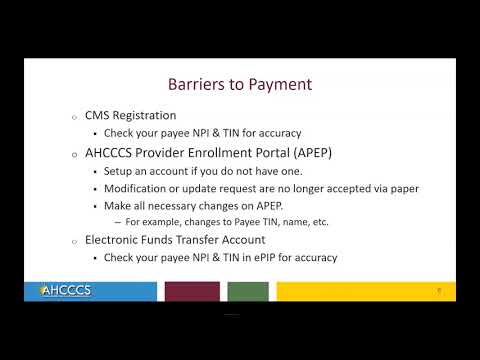
Open Forum: Objective 7 Health Information Exchange – June

PI Program Webinar: Open Forum: Objective 1 Patient Health Information & Objective 8 Public Health & Clinical Data – May
- Security Risk Analysis Requirements Tip Sheet_2021
- Final Frequently Asked Questions – Program Year 2021 Public Health
- Tips for Completing a Security Risk Analysis_2021
- Frequently Asked Questions – Program Year 2021 Stage 3
- AHCCCS Security Risk Analysis and Public Health Objectives Open Forum Presentation
PI Program Webinar: Open Forum 2021 Checklist – April

PI Program: Documentation Retention – March
- AHCCCS Program Year 2021 Documentation Webinar Presentation
- Frequently Asked Questions – Program Year 2021 Documentation Requirements
- Program Year 2021 – Documentation Retention Tip Sheet
PI Program: Electronic Clinical Quality Measures (eCQMs) for Meaningful Use – February
- AHCCCS Program Year 2021 Clinical Quality Measures Presentation
- Program Year 2021 Clinical Quality Measures – FAQ

PI Program Objective 7: Health Information Exchange – Summary of Care Instructions for Referrals/Transitions – February
- Promoting Interoperability (PI) Program – Facilitating a Transition of Care via the HIE 2 11 2021
- Frequently Asked Questions
Program Year 2021 Stage 3 Objectives for Meaningful Use – January
- AHCCCS Program Year 2021 – Stage 3 Presentation
- Frequently Asked Questions – Program Year 2021 Stage 3

2020 PI Program Webinar Series
PI Program Webinar: Program Year 2020 Documentation Retention – November 2020
- Final AHCCCS Program Year 2020 Documentation Webinar Presentation
- Final Frequently Asked Questions – Program Year 2020 Documentation Requirements
- Final Program Year 2020 – Documentation Retention Tip Sheet
PI Program Webinar: PY2020: Electronic Clinical Quality Measures for MU (eCQMs) – October 2020
- AHCCCS Program Year 2020 Clinical Quality Measures Presentation
- Final Frequently Asked Questions – Program Year 2020 Clinical Quality Measures
PI Program Webinar: Obj. 7: HIE Summary of Care Instructions for Referrals/Transitions – Sept. 2020

PI Program Webinar: Objective 8: Public Health and Clinical Data Registry Reporting – September 2020
- Final AHCCCS Public Health and Clinical Data Registry Presentation
- Final Frequently Asked Questions – Program Year 2020 Public Health
- Promoting Interoperability and ADHS Public Health Reporting Registries
PI Program Webinar: PY2020 Stage 3 Requirements Objective for Meaningful Use – August 2020
- AHCCCS Program Year 2020 – Stage 3 Presentation
- Frequently Asked Questions – Program Year 2020 Stage 3

PI Program Webinar: Open Forum for Meaningful Use – August 2020

PI Program Webinar: PY 2020 Objective 5: Patient Electronic Access Objective for Meaningful Use – July 2020

PI Program Webinar: PY2020 Security Risk Analysis for Meaningful Use – July 2020
- Security Risk Analysis Presentation
- Protect Patient Health Information: Security Risk Analysis Requirements Tip Sheet
- Tips for Completing a Security Risk Analysis (SRA)

PI Program Webinar: Objective 7: Health Information Exchange – June 2020

PI Program Webinar: Objective 2: Electronic Prescribing, Objective 3: Clinical Decision Support and Objective 4: Computerized Provider Order Entry – June 2020
- AHCCCS Electronic Prescribing, Clinical Decision, Computerized Provider Order Entry Presentation
- AHCCCS Electronic Prescribing FAQs
- AHCCCS Clinical Decision Support FAQs
- AHCCCS Computerized Provider Order Entry FAQs

PI Program Webinar: Objective 6: Coordination of Care through Patient Engagement – May 2020
- AHCCCS Coordination of Care through Patient Engagement FAQs
- AHCCCS Coordination of Care through Patient Engagement Presentation
Objective 8: Public Health and Clinical Data Registry Reporting – May 2020
PI Program Webinar: Objective 8: Public Health and Clinical Data Registry Reporting – April 2020

PI Program Webinar: PY 2019: Stage 3 Objectives for Meaningful Use – March 2020
- Download AHCCCS Program Year 2019 – Stage 3 Presentation Slides
- Frequently Asked Questions (FAQs) – Program Year 2019 Stage 3

PI Program Webinar: Objective 5: Patient Electronic Access to Health Information – February 2020
- Frequently Asked Questions – Clinical Quality Measures
- Download AHCCCS Clinical Quality Measures Presentation Slides
PI Program Webinar: Clinical Quality Measures (eCQMs) for PI Program – January 2020
- Download AHCCCS Documentation Retention Presentation
- Documentation Retention Tip Sheet
- Report Layout for Medicaid Patient Volume
- Report Layout for Needy Patient Volume

- Final Frequently Asked Questions – Program Year 2020 Documentation Requirements
- Final Program Year 2020 – Documentation Retention Tip Sheet
- Frequently Asked Questions – Program Year 2020 Stage 3
- Patient Electronic Access FAQs
- Protect Patient Health Information: Security Risk Analysis Requirements Tip Sheet
- Tips for Completing a Security Risk Analysis (SRA)
- AHCCCS Health Information Exchange FAQs
- AHCCCS Coordination of Care through Patient Engagement FAQs
- Frequently Asked Questions (FAQs) – Program Year 2019 Stage 3
- Frequently Asked Questions – Clinical Quality Measures
- AHCCCS Electronic Prescribing FAQs
- AHCCCS Clinical Decision Support FAQs
- AHCCCS Computerized Provider Order Entry FAQs